Match Day 2021
#SGUMatch
The best way to take part in the celebration is through using our hashtag—#SGUMatch.*
Simply add it to your post. It will appear on this page, and by clicking on it on any social media channel, you and your classmates will see the excitement that’s going on around you.
*By using our hashtag, you are giving us permission to share your photo. Due to privacy concerns, we do not recommend sharing the hospital that you matched at.
[ff id=”8″]
A Message from Faculty and Staff
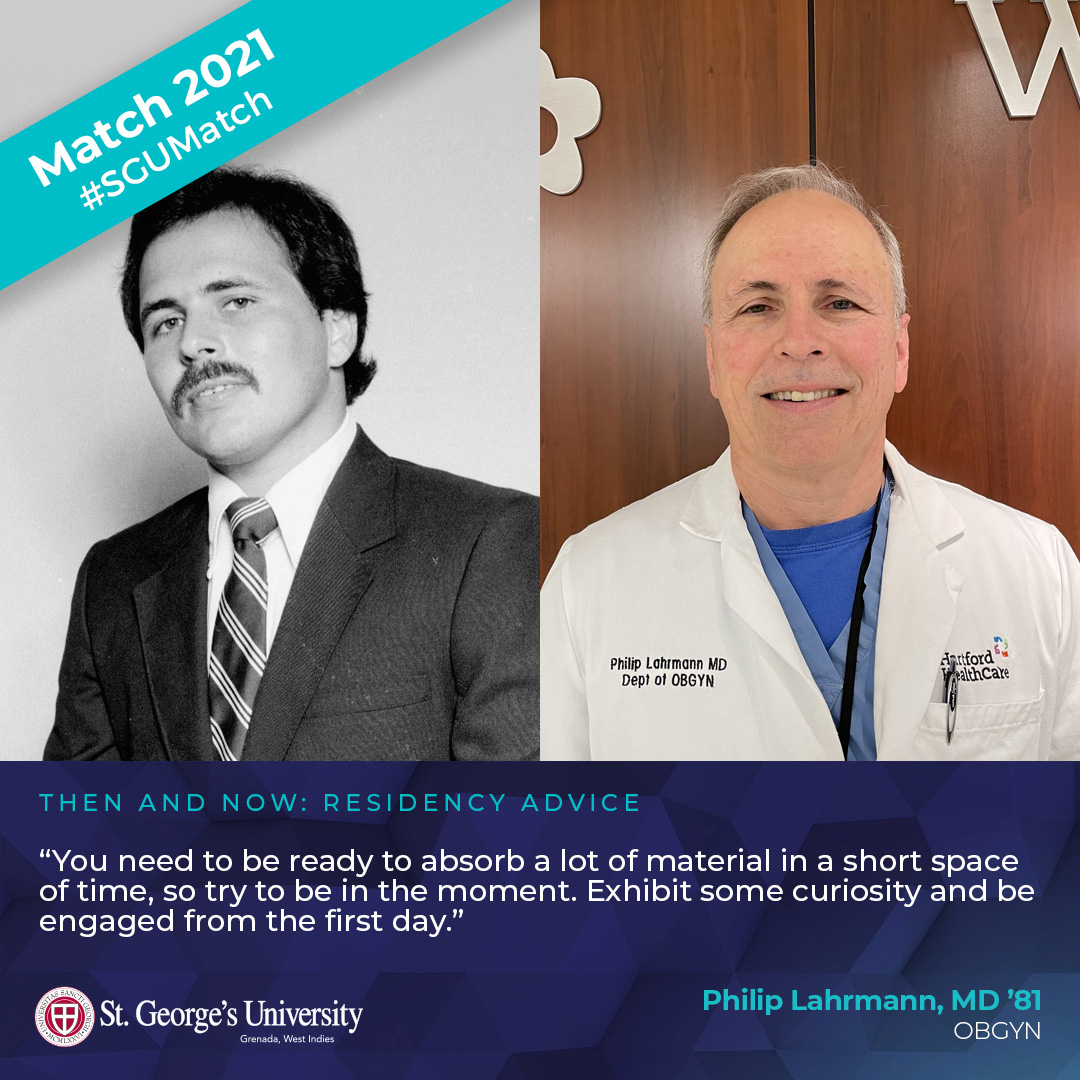
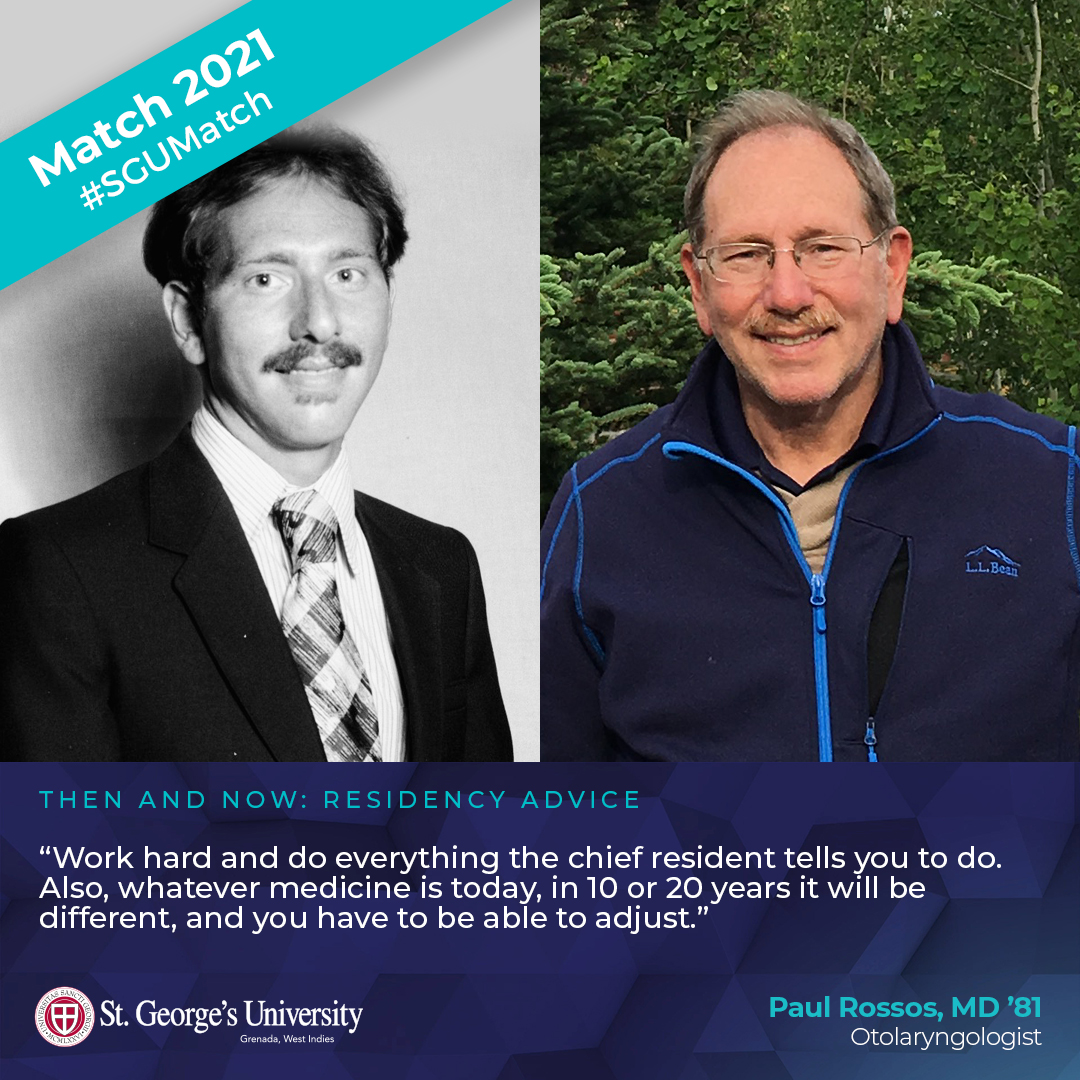
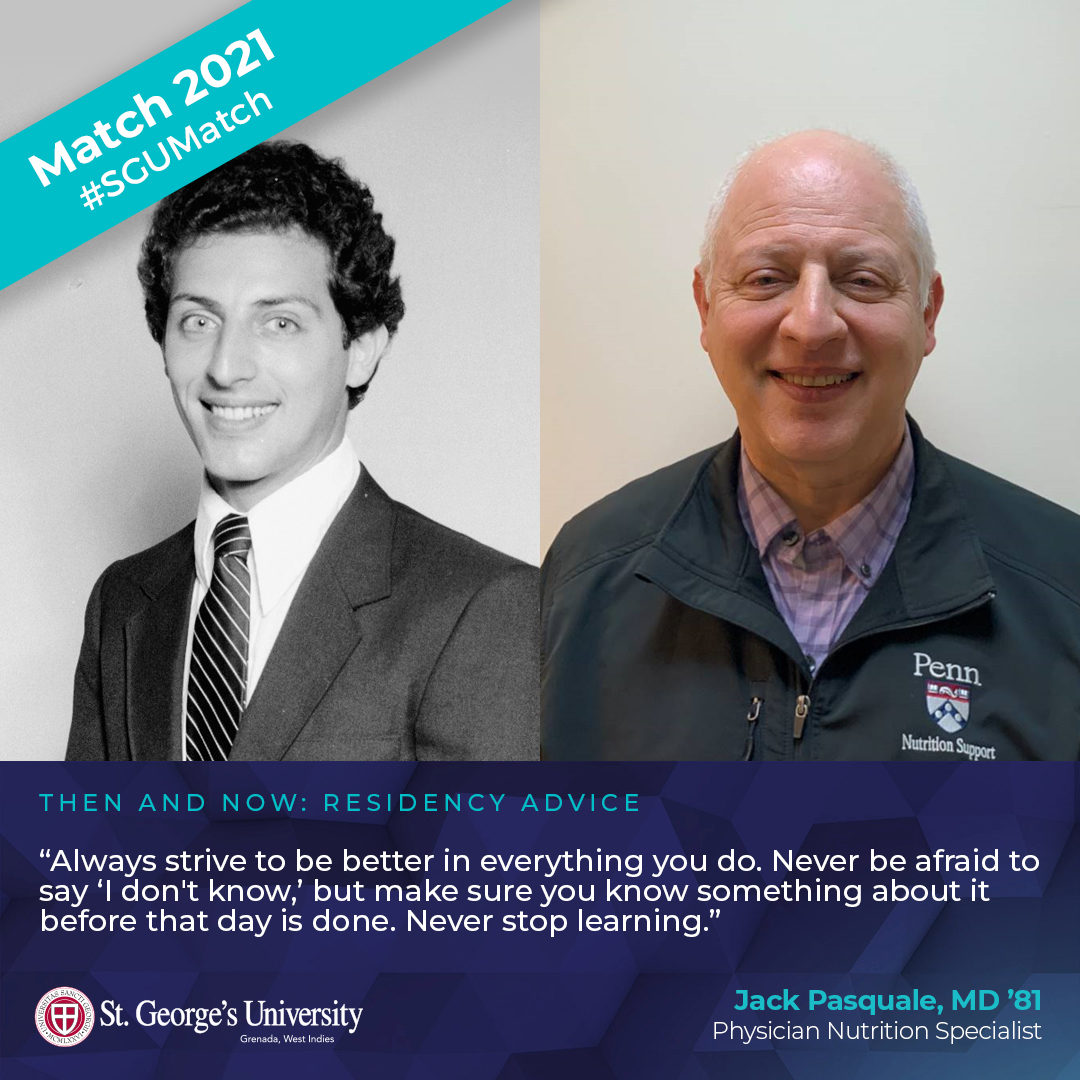
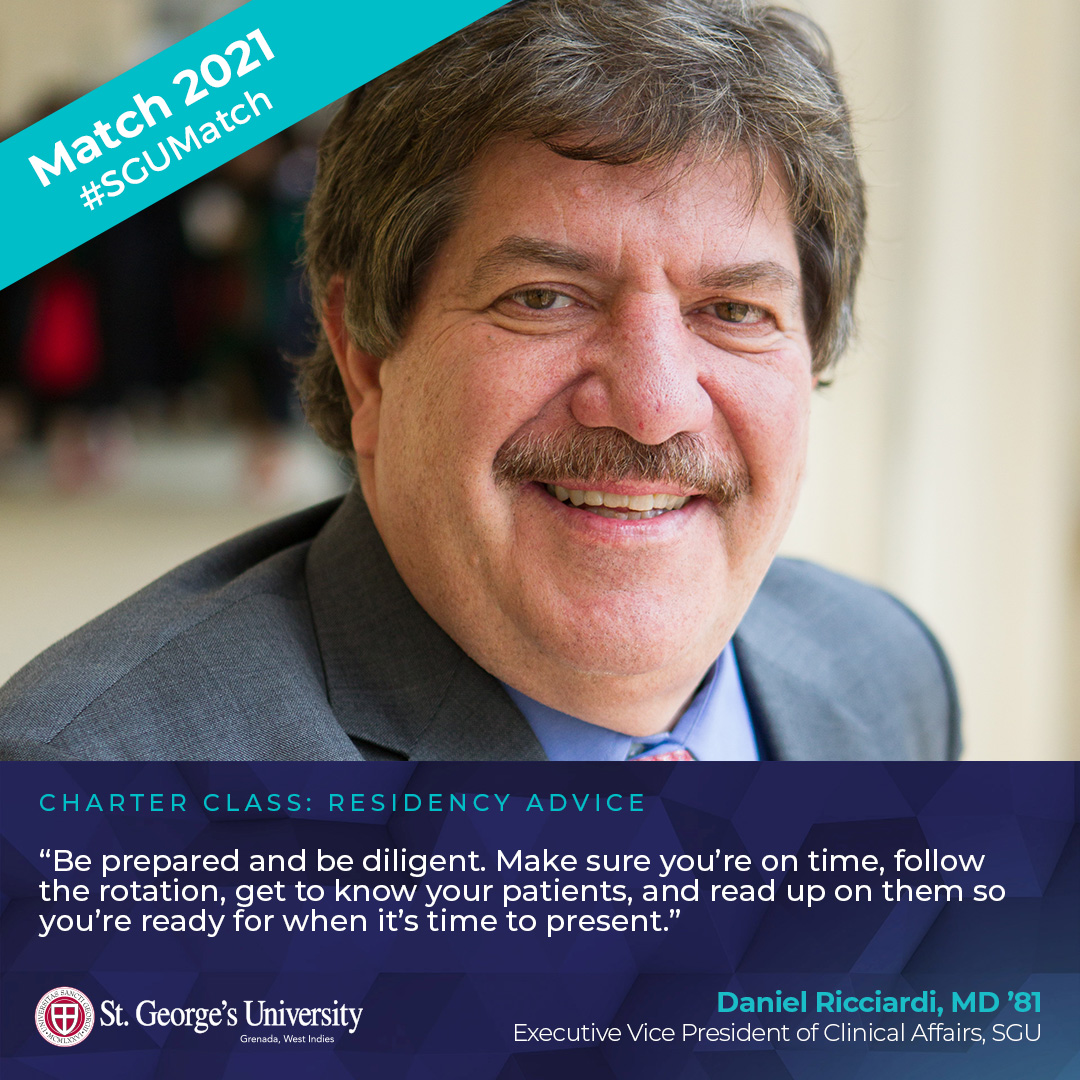
Thoughts and Advice from SGU’s Charter Class
Class of 1981
40 Years of Experience
Residency Advice
Downloads
Share your exciting news using one of our Match Day signs and we’ll retweet/share
your posts on social media and on this page. Be sure to use the hashtag #SGUMatch.
Print it, fill it, and post it.
Use Our GIFs Too!
Search terms like #MatchDay #SGUMatch
#SGU #StGeorgesUniversity #Doctor #MD
to use these on Instagram Stories.
Playlist & Virtual Backgrounds
To use the Zoom backgrounds, click directly on the image to enlarge and then right click to save the image. Upload to Zoom as a background. Backgrounds can also be found in the downloadable signs file.
SGU professor looks back on one year combating COVID-19

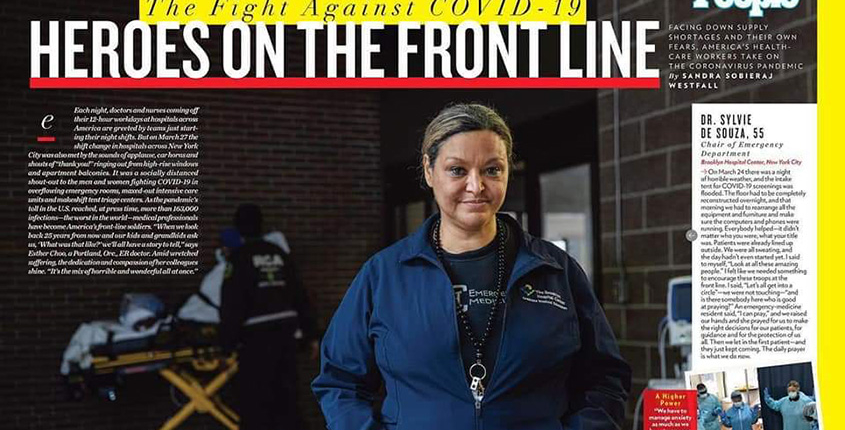
Dr. Sylvie de Souza (front) and the emergency medicine team at The Brooklyn Hospital Center in New York. Photos provided by Sylvie de Souza
Dr. Sylvie de Souza, director of emergency medicine at The Brooklyn Hospital Center (TBHC), and a clinical assistant professor for St. George’s University, was on the front lines when it all began. The day was March 1, 2020, when the first COVID-19 case was reported in New York City.
As the coronavirus spread throughout the city, putting pressure on the people and the mechanisms to treat ill patients, she remembers as much about what happened as the way it made her and her colleagues feel. It reminded her another catastrophic event—September 11, 2001.
“We immediately went into preparedness mode while the memory of 9/11 lurked in the back of our minds,” Dr. de Souza said. “Although the nature of the event was different, we all sensed that something major and perhaps terrible was about to happen. The anxiety of the unknown heading our way was palpable.”
A year later, Dr. de Souza reflected on the entire experience, how she and her team weathered the storm, and the hope she has for—and sees in—future SGU medical students who she trains for the fast-paced world of emergency medicine.
St. George’s University: How would you describe the past year in the emergency department at TBHC?
Dr. Sylvie de Souza: In September 2001, many of us remember standing by and watching New York’s bravest selflessly run into the burning building when everyone was running out, running toward the danger, into the fire, to save as many as they could. Sadly, when the unthinkable happened, we were the ones who went to the firehouses, like most New Yorkers, to praise the bravery and console the unimaginable loss. As emergency workers, there was not much else we could do other than what we had been trained to do: treat the walking wounded and the first responders. And we did, for weeks to come. Our lives were never directly endangered on 9/11.
This all changed in March of 2020 when the danger came directly at us. The fire came to us, and it grew uncontrollably with each day that passed. We stood in it, day after day, for hours on end, with little sleep, food, or drink, hardly recognizable in our plastic gear, trying to help as many as we could, with our own fear in the pit of our stomach, watching some of us fall, victims of the vicious enemy we were fighting. Many came to help in every way they could, but everybody knew, as we did, that this time around, it was as though we were the ones standing in the burning building, right there among the victims we were trying to save.
What an amazing twist of fate it was that, this time around, it was us New York’s bravest who came to clap for every evening. If anyone knew what we were feeling, I thought, it would be them. They clapped with the rest of the bystanders, a daily incantation of sorts, to harness the courage they knew we needed to keep going.
SGU: How did 2020 change you as a physician?
Dr. de Souza: I once read this sentence in a French publication. I do not recall who the author is, but it stayed with me: “Courage does not consist of doing the work that is expected of you; that is competence. Real courage is to conquer one’s fear and see the duty before the effort.”
I cannot recall a time in my entire career when this sentence rang truer or when I was, along with my colleagues, tested to honor the oath we had taken to come to the aid of others. It took all we had to overcome our own fears. We worked endless days and nights, not knowing what the fate of our patients would be, or our own, instead trusting that we were doing exactly what we were supposed to do—to follow our calling and answer the call of duty.
Many lessons were learned in the face of such adversity and uncertainty: 2020 was a year of great loss, but also a year filled with a sense of community, resilience, and hope. I face 2021 with a renewed sense of purpose and the knowledge that preparedness and togetherness are likely the most important tools we possess to confront adversity.
SGU: In what way has your role changed the most during the pandemic?
Dr. de Souza: With the restrictions imposed by NYC Department of Health at the beginning of the pandemic, no visitors were allowed in the hospital. Those measures were in place to protect those who were not yet infected.
As a result, we were no longer simply caregivers to the growing number of critically ill patients. We suddenly became their only “visitors,” their only connection to the outside world and their loved ones, their consolers, their prayer partners, their only and sometimes last human interaction, and most poignantly, the last ones to hold their hands as they slipped into unconsciousness or died. No amount of training could have prepared us to take on a responsibility of that scale. Watching patients die deprived of their loved ones or making their hastened last goodbyes on a video monitor was almost too much to bear.
Surrounded by all this despair and grief, we became closer as a team; we suddenly felt responsible for one another and supported each other through each day. As emergency workers, we had always known the importance of functioning as a team. This time, however, there was a whole new twist. We were now a team who had to operate in constant danger, facing mortality, that of those we cared for … and our own. We shared the same fears about our own unpredictable fate, fighting this vicious invisible enemy, not unlike a platoon sent to combat.

The Brooklyn Hospital Center. The oldest hospital in Brooklyn was one of many in New York City to combat the emerging COVID-19 crisis.
SGU: What can St. George’s University students rotating with the TBHC EM department expect to learn?
Dr. de Souza: Several faculty, myself included, partake in the weekly didactic conferences for EM residents and medical students. Our program has a dedicated clerkship director who organizes a series of didactic sessions and workshops where students receive direct feedback from the faculty. Aside from some exposure to a series of common complaints, medical students rotating through our department will leave the clerkship with a basic knowledge on the approach to the undifferentiated patient and introductory skills for the rapid recognition of the critically ill patient. We also place a lot of emphasis on the ability to communicate and function effectively in a team.
“As emergency workers, we had always known the importance of functioning as a team. This time, however, there was a whole new twist.”
SGU: Is there a personality trait that you find to be common among SGU medical students?
Dr. de Souza: I have had the pleasure of working many SGU students who rotated through our department over the years. Several of them became some of our most stellar residents. I have found them to be driven, focused, and resilient. Most salient is their overall ability to adapt and make the best out of any situation.
SGU: What is one piece of advice that you would give to a student who was considering a career in emergency medicine?
Dr. de Souza: During your ED rotations, immerse yourself in the ED life and culture. Merge with the ED team. It’s not about anyone of us and it’s not about you; it’s about the patient. When the team wins, and you participated, you won. Don’t worry so much about having all the answers. Be perceived as a vibrant, passionate, and compassionate member of the team—someone who anyone would want by their side in the trenches.
– Brett Mauser
Get to Know Dr. Sylvie de Souza
Video produced by The Brooklyn Hospital Center
Under the Microscope: COVID-19 Vaccines in Grenada
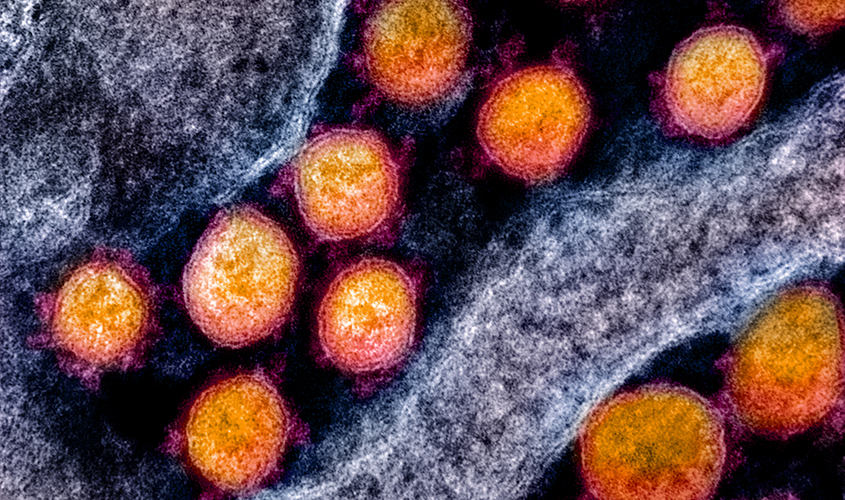
Dr. G. Richard Olds, president of St. George’s University, has committed his life to studying tropical and infectious diseases. All over the world, he has seen how viruses—these microscopic parasites that are invisible to the naked eye—can spread through a community, leaving damage in their wake.
One of the best methods to combat the virus is the use of vaccines. A version of the SARS-CoV-2 vaccine began being administered in Grenada last week, and a full program is currently being rolled out that places essential workers, elderly and Grenadian residents with pre-existing conditions on the priority list. Having long studied vaccines and their positive effect on healthcare, Dr. Olds is an ardent supporter of their implementation.
“I got my first COVID vaccine today,” he said.
Dr. Olds shed light on the vaccine that is currently being distributed in Grenada, what citizens can expect when receiving it, and the long-term outlook for COVID-19 in the country.
St. George’s University: What vaccine does Grenada currently have in stock? Is it being administered elsewhere in the world and how does it compare to other versions?
Dr. G. Richard Olds: Grenada is currently using the AstraZeneca vaccine, which is currently being used extensively in England. It was developed in partnership with Oxford University. In contrast to the two vaccines being used in the US, it is a chimpanzee adenovirus that has had the message for the spike protein placed within it. This vaccine can’t make humans sick, but it induces a high level of protection against COVID-2. Just like the mRNA vaccines used in the US, this vaccine requires two doses but has the advantage of being stored in cold but not freezing environments.
SGU: How exactly does this vaccine provide protection against SARS-CoV-2?
Dr. Olds: The COVID-2 virus attaches to human cells through a molecule on its surface called a spike protein. All current COVID vaccines target this molecule. Vaccinated people develop antibodies that block the binding of the spike protein to human cells. Unable to bind, the virus is unable to infect cells.
SGU: How long is the protection expected to last?
Dr. Olds: How long the vaccine will protect those who receive it is currently unknown, but it looks like all vaccines provide protection for at least a year and probably longer.
“If everyone doesn’t take the vaccine, we run the risk that COVID will circulate for a very long time.”
SGU: Is the vaccine available in one shot or does it require multiple shots over a period of time?
Dr. Olds: Most of the seven COVID vaccines require two shots, but the Johnson and Johnson vaccine only needs one shot. This is not currently available in Grenada. The interval between the two shots varies, but about a month is the most common. There are experiments in England now with the AstraZeneca vaccine with longer periods between the shots.
SGU: How safe is the vaccine that is available in Grenada? Are there any side effects?
Dr. Olds: All the COVID vaccines appear very safe. In blinded control studies, no difference was seen between vaccinated people and those that got sugar water in terms of long-term side effects. In the short run, vaccinated people will likely feel soreness in their arm, feel poorly for a few days, and may have a low-grade fever. None of these responses are serious, and they often respond to over-the-counter medicine.
The AstraZeneca vaccine currently in Grenada does not seem to cause severe allergic reactions. All minor reactions to the vaccine appear more commonly in reaction to the second vaccine, and are a sign that they are working.
SGU: Are there any pre-existing conditions that would prevent someone from getting it?
Dr. Olds: If a person is severely immune compromised—such as being infected with the AIDS virus, on high-dose steroids, getting chemotherapy, or having an organ transplant—they should consult a doctor before getting the vaccine.
SGU: Once an individual receives the vaccine, how will restrictions change for them?
Dr. Olds: Even after you get fully vaccinated, people will still need to wear a mask and socially distance until everyone on the island is vaccinated. That’s because vaccinated people are protected from dying from COVID, but they could still transmit the virus to others. Once everyone is vaccinated, life should return to normal.
SGU: Do you believe that all eligible individuals should receive the vaccine?
Dr. Olds: Everyone over 18 years of age should get the vaccine. Soon we will know if children over 12 should get the vaccine. The vaccine is very safe, and COVID can lead to serious illness or fatalities. In addition, COVID can cause long-term health issues for people. By now, millions of people in England have already received the vaccine currently available in Grenada without a problem.
If everyone doesn’t take the vaccine, we run the risk that COVID will circulate for a very long time, and the more the virus circulates, the greater the chance that a new variant will develop that the vaccine will not protect people from. It’s a race, and I hope this time humans win.
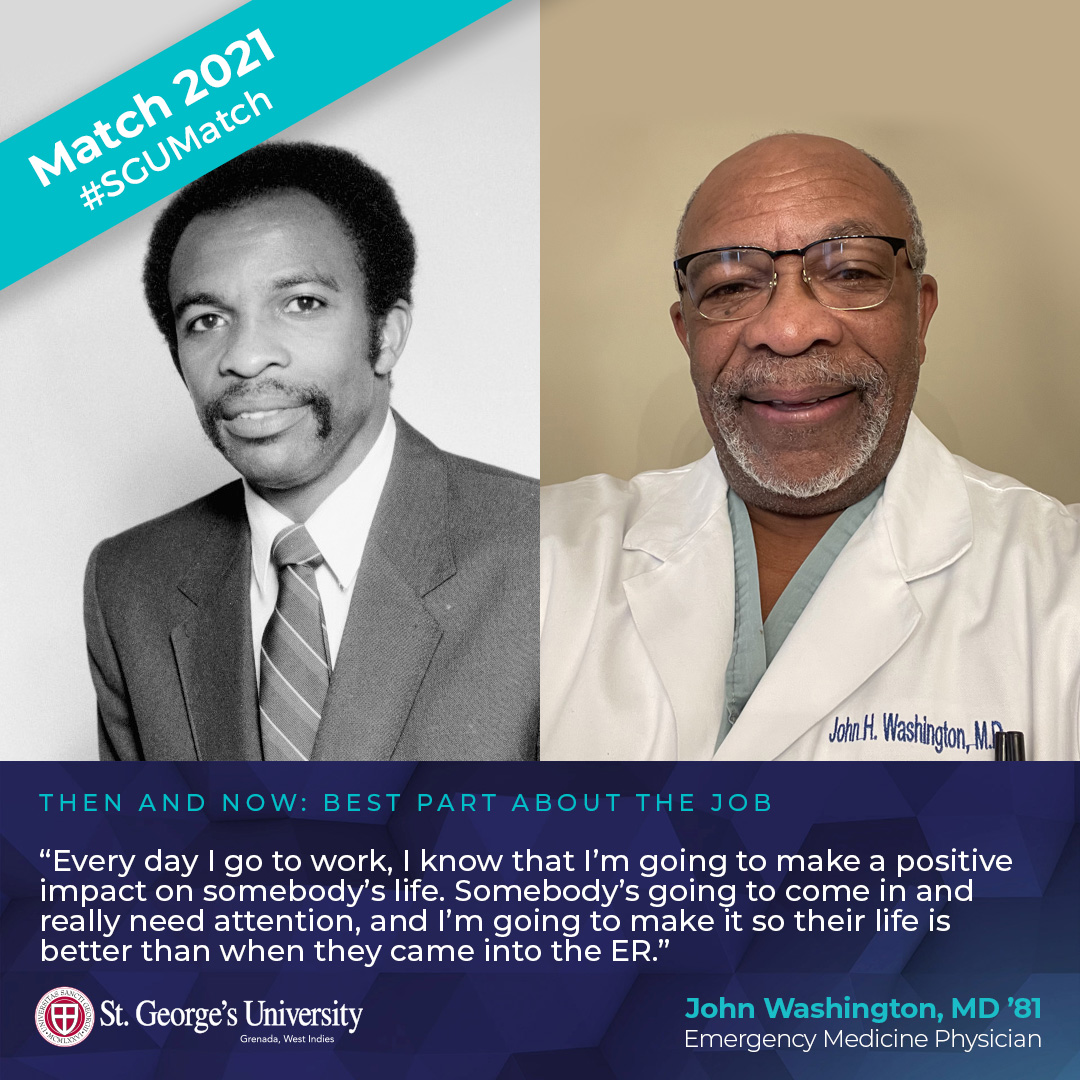
For First Black Graduate, SGU Was “Opportunity Of A Lifetime”
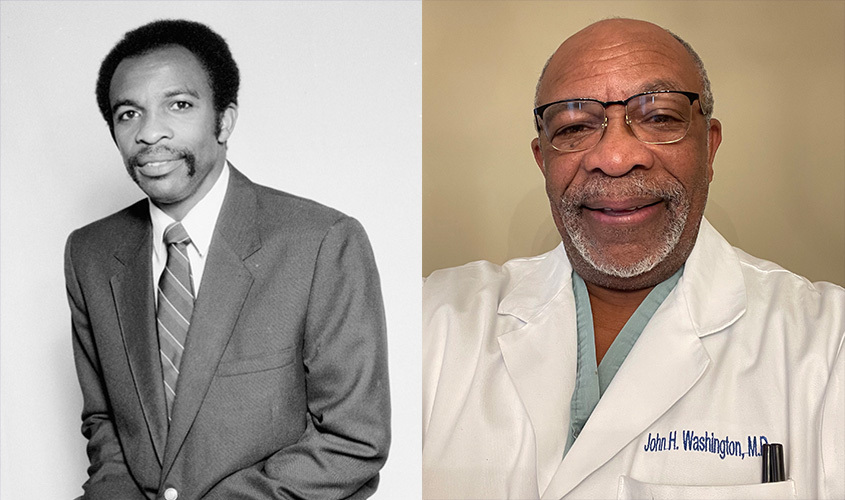
SGU News caught up with John Washington, MD ’81, who with his charter class colleagues were the first to enter medicine as St. George’s University graduates. Dr. Washington has spent the last 35 years working as an emergency medicine physician in Macon, GA, and he looks back fondly on where his journey began.
St. George’s University: How did you end up choosing SGU?
John Washington: Going to SGU was the opportunity of a lifetime for me. We’re talking about a time when black individuals didn’t really have that kind of opportunity in medicine. For us, we had to go to Howard or Meharry, which is the oldest black medical school in the nation. Some schools weren’t letting black medical students in.
A friend of mine at one school told me some stories about how he was treated—and of the things that went on. It’s amazing he made it through. He isn’t alone either. When I compared my time in Grenada to the experience that he and others had elsewhere, it was completely different. SGU was a great fit for me.
SGU: How would you describe the camaraderie amongst the charter class?
Dr. Washington: The most important thing I remember is that everybody stuck together. It was a tight-knit group, and everybody helped each other out in any way they could. We studied hard, and it was easy to see who was committed to making it through and building a legacy for the school. Looking back at it now, we were able to lay the groundwork for what was then this completely new and unique school.
SGU: What’s it like for you looking back on the foundation that you and your classmates built?
Dr. Washington: It’s just been marvelous. I believe that SGU is the preeminent foreign medical school in the world, in terms of the training it provides and the opportunity it gives students to practice in the US. Graduates from SGU are everywhere now, and they’re doing well. I’m proud to have been part of the first class and to have helped physicians who followed in our footsteps.
– Brett Mauser
SGU Celebrates Alumnae Impact On National Women Physicians Day
In honor of National Women Physicians Day, St. George’s University’s School of Medicine Alumni Association (SOMAA) held a virtual panel discussion to celebrate its accomplished alumnae making a difference every day in the medical community. The group of esteemed panelists delved into an open and informative discussion about their perspectives on not only being a woman physician but also the impact that female leaders can have on their organizations, as well as the impact those leadership roles can have on the women who hold them.
“I’ve learned to become a servant leader and a collaborative leader,” stated Gina Puglisi, MD ’87, attending adult hospitalist for Envision Physicians in New Jersey and regional medical director of hospital medicine for NEOU. “I’m a leader that gives to their team and makes sure their team is always happy. Everything I do is for the team because if the team is happy then the patients are happy.”
As a physician working in emergency medicine for the past 31 years, Dr. Puglisi has been in a leadership position since her third year out of residency.
“Most studies show that servant leadership and collaborative leadership are the most successful types of leadership,” added Dr. Puglisi. “As a servant leader, I do everything I can to make things easier for my team on a day-to-day basis so, that they can spend more time at the bedside with patients and less time getting bogged down with other aspects of their jobs.”
In addition to sharing their personal stories about the unique qualities that women leaders and physicians bring to the table—and some of the barriers they’ve faced along the way—the panelists also shared insights on how to balance their careers with their personal lives, wellness, and other passions and hobbies they may have.
“Achieving work/life balance is a continued work in progress,” said Marie Raphaelle Jean, MD ’09, a pediatric gastroenterologist at the University of Arizona. “No one has it completely figured out. However, what has served me well is that I became non-negotiable with giving life to activities that brought balance to my mind, body, and spirit. When I focus on those three things, it keeps me grounded.”
“Another good way to strike that balance is that when one vacation ends, start scheduling your next one so that you prevent burn out,” she added. “And lastly, remind yourself that you didn’t get to this place by chance. We have been vetted and we absolutely belong where we are and deserve to be where we are.”
With St. George’s University being the second largest source of physicians for the entire US workforce, the SOMAA was proud to host the online event acknowledging its female doctors who continue to provide excellent care and are committed to making a difference in the lives of their patients every day. The five SGU graduates on the panel represented a variety of specialties, including gynecology, radiology, emergency medicine, internal medicine, and pediatrics.
“It’s impossible to not be inspired by these women physicians—their stories and their impact on healthcare,” said Robert Alig, vice president of alumni affairs at St. George’s University. “It’s incredibly powerful to hear them speak and to connect their experiences back to their education here at St. George’s University. It’s unmistakable that they care deeply about their profession, one another, and about SGU, but most important is their commitment to educating themselves, their peers, and their colleagues to make a difference in healthcare.”
– Ray-Donna Peters
Canadian Grad Secures Highly Competitive EM Fellowship

The journey for Ryan Toews, MD ’19, has taken him from an international medical school experience, to his top-choice residency back in Canada, and now, to a much sought-after emergency medicine fellowship beginning this summer.
Dr. Toews was ecstatic to learn that he had secured one of only a few such fellowship positions through Canada’s Family Medicine Enhanced Skills Match, and that he’ll remain in the U of S system, just a short drive east from where he trained in Swift Current for residency. He received his nursing degree from the University of Calgary before joining the St. George’s University of Grenada School of Medicine/Northumbria University Four-Year Program, for which he spent the first year of basic sciences in Newcastle, United Kingdom.
SGU News connected with Dr. Toews to learn what captured his interest in the fellowship position, and his hopes for the future.
St. George’s University: What prompted you to apply for this fellowship position in particular?
Ryan Toews: I was drawn to the opportunity to further develop my acute care skills in order to provide a high quality of care to patients in a wide variety of settings.
SGU: What does this fellowship position mean for your future?
Dr. Toews: It will mean that emergency medicine will be a large focus of my career, as well as the provision of acute care medicine. I hope this leads to an improved and versatile skillset that will allow me to practice in rural, regional, and urban settings.
SGU: How would you describe your residency experience at the University of Saskatchewan?
Dr. Toews: Building on skills learned from clerkship, residency has been a very positive experience with a faculty dedicated to teaching and cultivating clinical knowledge. I have been able to apply my clinical skills to a variety of different patient populations in a variety of different settings.
SGU: How did SGU prepare you for residency and the next step in your career?
Dr. Toews: SGU created a solid foundation as well as engrained a strong work ethic that has allowed me to be successful in both residency and fellowship.
– Tornia Charles
SGU Alum Featured in New York Times and US News & Health Report

Dr. Andrew Carroll, MD ’96, a family physician and primary care doctor in Chandler, AZ, was recently featured in both the New York Times and US News & Health Report, offering his perspective on COVID-19 vaccinations, as well as the intricacies of life as a family medicine physician.
In the Times article, “Doctors’ offices contend with a deluge of requests for the vaccine,” Dr. Carroll, who was recently re-elected to the board of directors for the American Academy of Family Physicians (AAFP) for 2020-21, said patients who were hesitant about receiving the vaccine may feel more comfortable if it was given by their primary care physician.
“Many patients are very reluctant to get a vaccine that doesn’t have a proven track record,” said. “They’d rather get the vaccine from somebody they can call right afterwards if they’re having problems.”
In “How to Become a Family Medicine Physician” by US News & Health Report, Dr. Carroll described what it’s like to be a family medicine physician.
“Family medicine is the only singular medical specialty which is tasked with taking care of all people at all ages,” said Dr. Carroll. “We are, in a lot of ways, the Swiss Army knife of all specialties.”
Dr. Carroll is passionate about family medicine. SGU News profiled Dr. Carroll following his election onto the AAFP board in 2019.
“The grassroots family physician hasn’t been heard loud enough,” Dr. Carroll said at the time. “I want to be that loud voice.”
– Laurie Chartorynsky
9 Questions with MD Student Ololade Akinfemiwa

Ololade Akinfemiwa, MD ’21 (expected), is enjoying her challenging internal medicine rotation as a fourth-year student at a clinic affiliated with Kingsbrook Jewish Medical Center.
Originally from Toronto, Canada, she chose St. George’s University because, after speaking with a number of graduates practicing in the US and Canada in various specialties—all encouraged her to apply. “I am glad I did,” she said.
Hoping to inspire more black women to go into medicine, Miss Akinfemiwa is active within the Student National Medical Association (SNMA), serving as vice chair of the national chapter’s Community Service Committee. SNMA is committed to supporting current and future underrepresented minority medical students by addressing the needs of underserved communities, and increasing the number of “clinically excellent, culturally competent, and socially conscious physicians.”
Get to know Miss Akinfemiwa below.
1. What are you learning right now in your internal medicine rotation?
Ololade Akinfemiwa: I am currently on an outpatient rotation and I am learning the importance of effective communication of health-related information. It makes a huge difference when patients have a good understanding of their medical conditions and how to manage them.
2. What is the most surprising or exciting lesson/case learned while in clinical rotations?
Akinfemiwa: I saw a patient with Lyme disease with the classic rash that looks like a bull’s eye. I had so many questions about it and was excited to actually see it in person.
3. Do you plan to go into primary care or specialize?
Akinfemiwa: I plan on going into emergency medicine and I have an interest in global health.
4. Favorite rotation/elective so far?
Akinfemiwa: Emergency medicine, of course!
5. What do you miss most about Grenada?
Akinfemiwa: I miss the warm weather, beaches, and Umbrellas Beach Bar.
6. What has been the most challenging part of clinicals?
Akinfemiwa: Right now, the most challenging part of clinicals has been seeing the devastating effects of COVID firsthand.
7. What has stood out to you most about the role of physicians during this pandemic and how has it affected the type of doctor you aspire to be?
Akinfemiwa: This pandemic has highlighted the need for more doctors and revealed the vulnerabilities in the healthcare system. Knowing that things could have gone better has only inspired me to be a part of making that possible.
8. February 3 is National Women Physicians Day. What does it mean to you to be a black woman about to enter the medical field? What do you hope to accomplish as a doctor?
Akinfemiwa: Black female doctors represent only about 2 percent of physicians in the US. I decided to go into medicine to help fight for health equity. I hope to inspire more black women to pursue medicine because we are truly needed. Black physicians are essential to achieving equity in medical care and I look forward to supporting and advocating for patients as an emergency medicine physician.
9. Best piece of advice about clinical rotations for basic sciences med students?
Akinfemiwa: Take care of yourself and listen to your body. If you love to take naps like me, take those naps!
— Laurie Chartorynsky
Prioritizing Student Support During Clinical Rotations: Faculty Spotlight on Associate Dean Dr. Sherry Singh

This month’s faculty spotlight is on Dr. Sherry Singh, a 2000 graduate of St. George’s University and associate dean of SGU’s US clinical studies program. She also is the director of the US Onsite Clinical Student Support Program.
In her current role, Dr. Singh has her hands in many facets of the clinical student’s journey to graduation, including visiting SGU’s clinical sites, overseeing curriculum, ensuring academic standards are met, as well as participating in the development and implementation of clinical student support modalities. She also enjoys interacting directly with students to offer guidance as they navigate their clinical years.
Among the topics she discussed with SGU News—advocating for women in healthcare as well as the need for students to prioritize self-care during the COVID-19 pandemic.
St. George’s University: Navigating clinical studies is an important time. What advice do you have for students?
Dr. Singh: I consider the third year of medical school at SGU the toughest year of their medical studies but also the most rewarding as they apply their basic sciences knowledge directly to patient care.
The third year will require a daily diligent commitment to learning both in the clinical environment as well as study time. I encourage students to keep an open mind as they approach each specialty and consider these years an opportunity to learn about all medical specialties, many of which they may not get a chance to experience directly once they enter into their chosen residency.
The fourth year is a time to strengthen their knowledge as they prepare to enter into residency. With such a tremendous network of clinical sites, I encourage students to take this opportunity to diversify where they do their electives.
SGU: You are a strong supporter of student wellness initiatives at SGU. Why it is important for medical students to take self-care seriously, especially during the pandemic?
Dr. Singh: “Wellness” has become somewhat of a buzz term in today’s world, yet it is not necessarily embraced by those in the world of medicine. As caregivers, it is very difficult to remember to care for yourself. With the pandemic adding yet another layer of complexity, physician burnout—and the number of healthcare workers as a whole—is on the rise. The perseverance with which our students have withstood these difficult times is a testament to their abilities.
Nonetheless, it is critical they manage their time and make self-care a priority—be it exercise, connecting with others, or learning and practicing mindfulness. Learning how to incorporate and build on these skills will lead to a more resilient physician in the long run. Students should take advantage of the various services SGU has to offer available via the University Portal (The Well and through BCS Group).
SGU: National Women’s Physician’s Day is Feb. 3. How has the landscape of medicine changed over the recent years for women physicians?
Dr. Singh: Women are now a majority in medical schools which is helping to balance the ratio of physicians in the workforce. As a result, there continues to be increased awareness of the issues that female physicians face, including work-life balance, compensation discrepancies, and gender equity. Women have taken on roles in both the medical world as well as in leadership positions to help fuel change. In addition, with increased awareness, more men are also helping to equalize the opportunities for men and women. As we recognize and continue to discuss the issues women in medicine face, it is imperative to develop amenable solutions to ensure their success and impact in healthcare.
St. George’s University School of Medicine Alumni Association will be hosting a virtual event to celebrate National Women Physician’s Day on February 3 at 9 pm ET. Students are encouraged to log on to the Facebook Live event that will be held simultaneously.
SGU: As part of the Advisory Council for the Women Business Collaborative, you recently hosted the first Healthcare Forum for WBC. What were some of the key takeaways from that discussion?
Dr. Singh: This was a very exciting opportunity to connect with several leaders in healthcare. With SGU being the largest provider of physicians to the US workforce, hosting this forum was a very important start for me.
Key points of discussion were:
- The ongoing need for mentorship for women (from both women and men), not just awareness but acceptance of the specific issues that women face in striving for work/parenting/life balance;
- The need to find ways to support women physicians in innovative ways and remove barriers so they can continue successfully as physicians as well as leaders in healthcare; and
- The positive impacts on patient care from women physicians.
SGU: How can female med students implement these lessons?
Dr. Singh: Our female students should continue to strive for excellence in all fields of medicine. I encourage them to seek out mentorship as well as lead the way for others toward their goals. Embracing diversity and inclusion and procuring a sense of belonging along the way are essential as we work toward a more equitable environment. This is true for all students, not just our female students.
SGU: How has your career in medicine influenced your role in academia?
Dr. Singh: My career in medicine has been a strong influence on my role in academic medicine by allowing me to bring my own experiences from my teaching roles in understanding the complexities that clinical students face and the particular skill sets they must develop. By understanding the practice of medicine in our ever-changing world, it has allowed me to contribute to the ongoing refinement of our clinical program at SGU with the goal of continuing the essential and positive impact our students continue to have in the US and around the world.
SGU: What is your best memory from attending SGU?
Dr. Singh: I am often reminded of the surreal excitement I felt as a student arriving in Grenada—in particular, at our White Coat Ceremony. Just as fondly, I recall the overwhelming feeling as I entered Lincoln Center in New York City for the commencement ceremonies with my classmates. Those friendships have long endured. For me, I not only get to pay it forward but to share those moments of excitement as I help new students put on their white coats and, during commencement, hood our deserving graduates. It is truly the best gift!
— Laurie Chartorynsky
1,000 Residency Slots Approved by Congress: What it Means for Medical Students

Congress recently passed a measure to fund 1,000 postgraduate residency positions over five years as part of the Medicare-supported program—the first increase in nearly 25 years according to the American Association of Medical Colleges (AAMC). St. George’s University President Dr. G. Richard Olds explained to SGU News what the increase means for our medical students. In addition, Dr. Olds also recently appeared on Action News Jax (Jacksonville, FL) to discuss the new medical residency funding in the stimulus package.
St. George’s University:  What does this mean for SGU medical students, especially those applying for residency?
What does this mean for SGU medical students, especially those applying for residency?
Dr. Olds: This new legislation should help our students in the Match no matter what specialty they decide to go into. Also, these new slots are permanent in contrast to the teaching health center funds that have to be renewed by Congress every few years.
SGU: What specialties will be included?
Dr. Olds: Potentially all specialties are included, but an institution can’t just expand specialty slots. Half must be for primary care, which includes OB/GYN.
SGU: Residency positions in rural and underserved communities were highlighted as a particular focus in the legislation. Why is that important?
Dr. Olds: The population is both growing and aging. The real problem, however, is a maldistribution of doctors geographically and a maldistribution of doctors by specialty. The first issue points out that affluent urban and suburban areas of the US often have a surplus of doctors, while underserved rural and urban areas have severe shortages. In big states, for example, the surpluses in affluent areas often mask the severity of shortages in rural and poor urban areas.
The second problem of maldistribution by specialty is created by the fact that 70 percent of US medical students specialize. The country needs over half to go into primary care fields. To make this issue worse, primary care doctors as a group are older, and age and COVID-19 are driving them into retirement faster than specialists.
SGU: How and why did these positions become available?
Dr. Olds: The issue that is causing problems in the physician pipeline are residency slots—not medical schools and students. Although there are far too few US medical schools for the current need, 25 percent of all residents in US residencies are international medical school graduates (such as SGU grads), and there are far more doctors who want to train in the US than we have residency slots to accommodate them. The shortage of graduate medical education (GME) slots is driven by a decision made in 1997 to cap GME funding by Medicare. Pressure has been growing to increase GME slots because of the growing doctor shortage. This is the first time in over 20 years that Medicare has increased the GME caps on most teaching hospitals.
While the number of additional residencies will not be enough to solve the doctor shortage in the US, and only a percentage of these slots will go to rural primary care residencies where they are most needed, it’s a start.
SGU: What is the rough number of Medicare-funded residency positions now, and why is adding these residency positions such an important breakthrough?
Dr. Olds: Medicare currently funds about 90,000 GME slots, the US Department of Veterans Affairs funds about 12,000, and children’s hospitals fund about 7,000 each year. Remember that training in internal medicine or pediatrics takes three GME slots spread over three years; general surgery five GME slots, etc., since you need a funded slot each year of your training. If you crunch the numbers, we have the ability to train about 35,000 new residents each year, mostly through the Match.
While the addition of 1,000 slots spans five years, and some of those slots will go to big teaching hospitals that are currently over their cap, it’s the first time in decades the number of Medicare slots have increased. It’s a big deal.
– Laurie Chartorynsky