Mother’s Cancer Battle Motivates SGU Grad to Become Breast Surgeon
 A doctor delivered the news—cancer, an aggressive form. Joseph Di Como’s mother, a cornerstone of the family, would have to undergo surgery and many months of treatment.
A doctor delivered the news—cancer, an aggressive form. Joseph Di Como’s mother, a cornerstone of the family, would have to undergo surgery and many months of treatment.
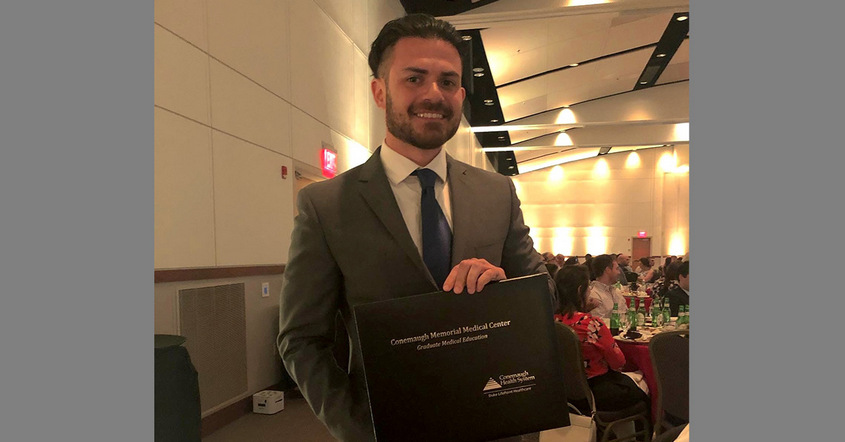
Her struggle changed the course of his life forever. More than 15 years later, now a doctor, Joseph Di Como, MD ’14, is providing important care and instilling hope in patients as a breast surgical oncology fellow at Brown University, Women and Infants’ Hospital of Rhode Island.
“Although I enjoyed all of my clinical rotations, surgery was the one that called to me the most, and even though I enjoyed every subspecialty of surgery, I felt that breast surgical oncology would give me the most personal satisfaction,” he said.
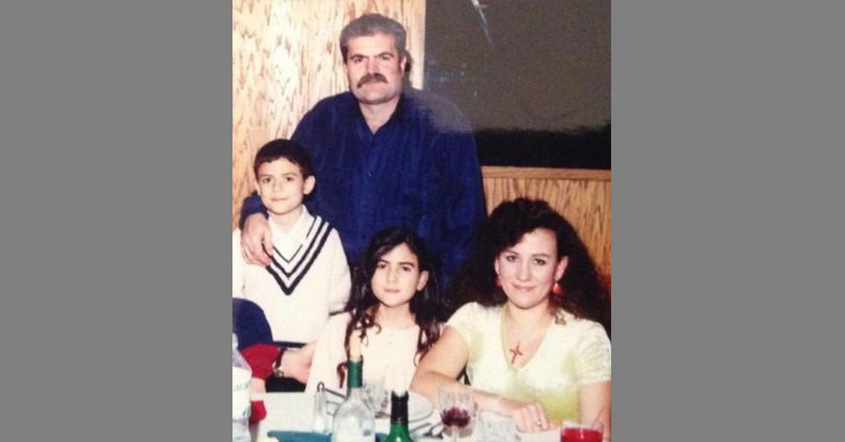
He was just a sophomore in high school when his mother learned that she had inflammatory breast cancer. The diagnosis blindsided the family. His mother was healthy, still young, and there was no family history of cancer.
“It was extremely difficult, as a young kid in high school, to juggle between school, extracurricular activities, and coming home to that situation every day,” Dr. Di Como said. “We were all optimistic at first, but as her health continually worsened and we learned more about what was going on during the different stages of the disease, it was very difficult for everybody.”
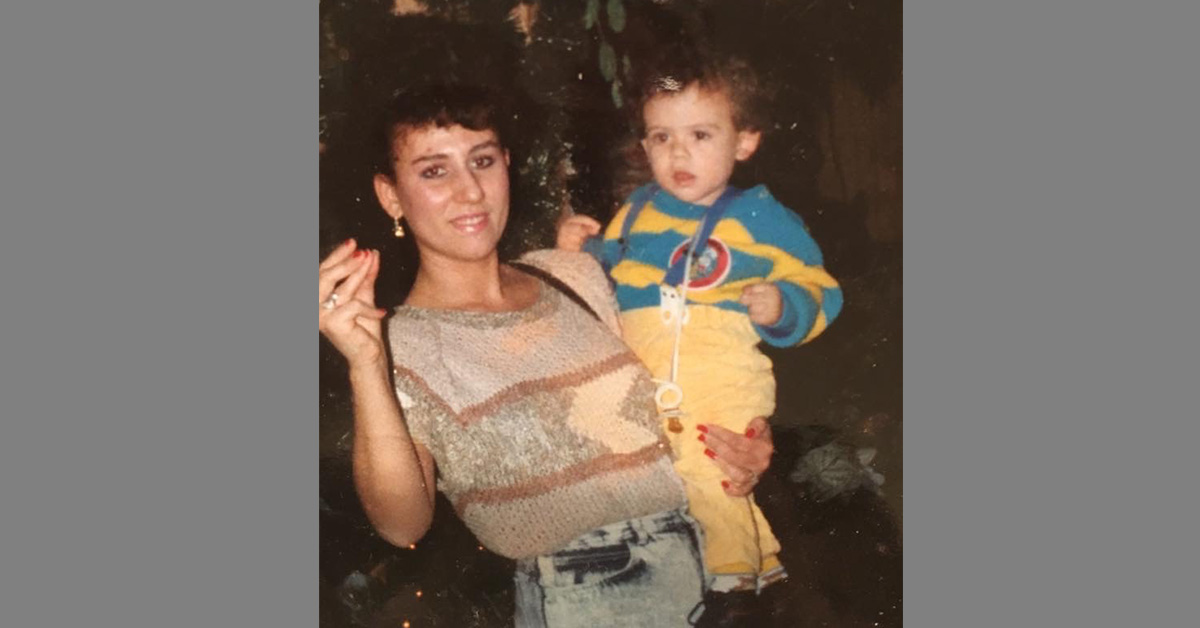
Antonina Di Como battled the disease for 16 months before passing away in November 2003 at age 44. Her death was the turning point for Dr. Di Como. He went from being an average student to a superior one—and his career path was clear.
“After that, I knew I wanted to be a doctor, specifically to treat cancer,” Dr. Di Como said. “I tried to keep an open mind throughout medical school, but I knew what I wanted to treat.”
Now fully immersed in cancer care, he works toward achieving positive results for patients in Rhode Island. Dr. Di Como operates on patients with both benign and malignant conditions, using the most up-to-date surgical techniques. He marvels at how these techniques are rapidly evolving and how treatment has become tailored for patients based on the biologics of a tumor. As a fellow, he preps patients for surgery or any extra imaging or testing they may need, and also co-coordinates a weekly tumor board, for which he and another oncology fellow present all new cancer patients or those with any benign masses or conditions for further workups.
“Different tumors behave differently, and different factors will direct how we tailor the therapy,” said Dr. Di Como. “It will depend on everything from a patient’s hormone receptor status and their reaction to chemotherapy to his or her age, medical comorbidities, and where they are in life. There’s no one cure that fits all.”
“A doctor’s job shouldn’t just be treating and curing disease; it’s about improving the life of a patient through empathy and compassion.”
In addition to his clinical responsibilities, Dr. Di Como is committed to conducting research to help progress oncology even further. Current projects include the use of radiofrequency identification (RFID) to tag breast cancers for surgical excision, in comparison to the standard use of wire localization in breast tumors, whereby wires mark lesion locations prior to surgery. Also, with the help of new technology, he conducts intraoperative angiograms using a florescent green marker to identify vessels in the patient’s breast prior to doing a mastectomy with reconstruction.
“By doing this procedure, our hope is to preserve these vessels to see if that has any impact on tissue viability and flap viability,” he said. “Having a flap that isn’t getting enough blood flow is one of the biggest and most detrimental complications a patient can have, so we’re trying new ways to avoid that, in order to help these patients that are undergoing reconstruction right after surgery.”
Each day, he is reminded of his family’s own encounter with breast cancer. It has changed him as a person and as a doctor, and has indirectly assisted the patients that he treats.
“I know how it feels to be on the family side of these diagnoses,” Dr. Di Como said. “Even if the prognosis is poor, it’s very important that, even if you cannot cure the patient, that we find a way to make everybody feel comfortable. A doctor’s job shouldn’t just be treating and curing disease; it’s about improving the life of a patient through empathy and compassion, to try to do everything you can to make the rest of their time here as comfortable and fulfilling as possible. Patients and their families are appreciative as long as they know that somebody cares, that somebody is on their side.”
He describes it as a “vital, sacred experience that cannot be underestimated.” With the care his own mother received, Dr. Di Como witnessed the kind of difference it can make for a family, and the experience has helped shape the rest of his life—and the lives of those he treats.
“Before she passed, I told my mom that I was going to be a doctor,” he said, “and I’m proud to say that I am.”
– Ray-Donna Peters
For more SGU coverage of Breast Cancer Awareness Month, check out Cancer Scare Inspires Grad To Become Oncologist At Memorial Sloan Kettering.









 Advocacy seems to come naturally for Andrew J.P. Carroll, MD ’96, founder, owner, and medical director of
Advocacy seems to come naturally for Andrew J.P. Carroll, MD ’96, founder, owner, and medical director of 








