Marine, Wildlife, and Conservation Biology Degree Gains Accreditation from Royal Society of Biology

St. George’s University School of Arts and Sciences (SAS) is pleased to announce that the Bachelor of Science Honors (BSc Hons) in Marine, Wildlife, and Conservation Biology (MWC) has been accredited by the Royal Society of Biology (RSB). It becomes the first program in the Western Hemisphere to obtain this distinction, further establishing SAS as a premier higher learning institution in the Caribbean.
The degree program is housed within the SAS’s Department of Biology, Ecology, and Conservation (BEC). It is only the 11th program outside of the United Kingdom to earn RSB accreditation, which will last through the end of 2026.
“We are very enthusiastic not only about the breadth of opportunities available in this program but also about its potential for current and future students,” said Dr. Lucy Eugene, dean of the SAS. “There is nowhere quite like Grenada for studying marine and terrestrial biology, and we’re so proud of what this program has become, and of all the incredible faculty and staff members who helped us attain this accreditation.”
This marks another accreditation by an international body joining other SGU programs:
- School of Medicine: Grenada Medical and Dental Council (GMDC)
- School of Veterinary Medicine: American Veterinary Medical Association (AVMA) and Royal College of Veterinary Surgeons (RCVS)
- SAS BSc Nursing degree: Grenada Nursing and Midwifery Council (GNMC) and the Caribbean’s Nursing Board
- Department of Public Health and Preventive Medicine Master of Public Health (MPH) degree: Council on Education for Public Health (CEPH)

“With this accreditation, our students can be confident that their program is consistent with internationally recognized standards and that they are prepared to undertake graduate programs,” said Dr. Cristofre Martin, chair of the Department of Biology, Ecology, and Conservation. “It also gives future employers and advisors confidence that their employees have been well trained in marine and terrestrial biology,”
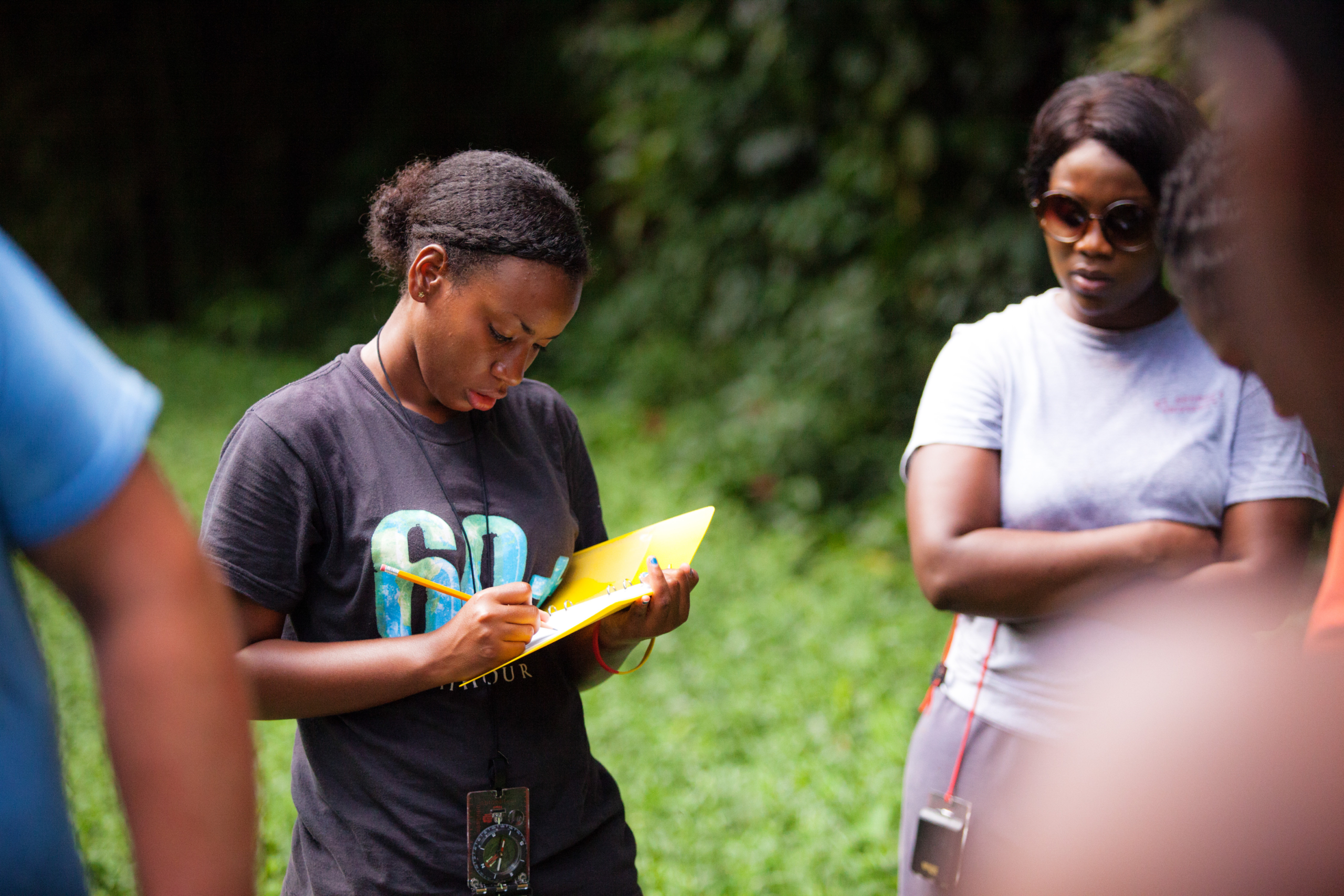
To graduate, students are required to complete 121 hours of coursework in lectures, the laboratory, and in the field, where they develop skills required to conduct ecological surveys, measure abiotic parameters, and manage and analyze data, while implementing a research design.
“Grenada is ideal to study marine, wildlife, and conservation biology,” said Dr. Patricia Rosa, BEC deputy chair and MWC program director. “It offers a unique learning environment considering our classrooms are rainforest, dry forest, mangroves, estuaries, freshwater, and ocean ecosystems. This diversity of ecosystems is also readily accessible; one can go from the beach to a mountain peak in the same day.”
“We’re so proud of what this program has become, and of all the incredible faculty and staff members who helped us attain this accreditation.”
All students must also complete an independent research project and a capstone thesis in their final year to graduate. Upon doing so, graduates receive an accredited honors degree and a certificate outlining the mastery of 75 technical skills related to marine biology, as well as transferrable job skills such as leadership, communications, and project management.
“This accreditation will lead to more opportunities and recognition for our students and graduates,” said Dr. Rosa. “It will also enable our department to enhance research capacity and train more highly qualified personnel for conservation in the Caribbean.”
What graduates are saying about the MWC program
Farihah Khan (Trinidad and Tobago), Class of 2019:
“I can confidently say that my time at SGU as a MWC student was well spent. The program’s high academic standards allowed me to develop a solid foundation in science and instilled in me a strong work ethic and sense of professionalism. Its Environment Conservation Outreach (ECO) student organization also encouraged me to balance academic work with extracurricular club activities. The rapport between students and educators was excellent and the teaching is unparalleled. It sets you on a positive trajectory as you enter the working world or continued studies.”
Saiyana Baksh (Guyana), Class of 2021:
“My experience at SGU has been no less than exceptional and enlightening. The University overall is challenging, and being an international student had additional challenges. SGU’s commitment to providing students with high academic and professional skills is constant and reliable. It has made me capable of handling anything that’s thrown my way. Their commitment to quality education allowed me to reach a level of maturity and wisdom that may not have been possible under different circumstances.”